There are those who want to make a plan for everything. There are those who simply arrive when they have time. That's basically the essence of the walk-in vs appointment controversy.
Appointments sound like the logical choice—schedule a time, arrive, get treated. But life is messy, and not everything happens on time. People are late, things take longer than expected, or someone doesn't arrive at all.
That’s where walk in appointment options can actually save the day.
If you’ve ever wondered what a walk-in appointment is or if it actually works better, this blog breaks it down and explores more about what helps service run smoother, for everyone.
Why Appointments Became Popular
Appointments became the default method in hospitals primarily because they make things feel more manageable. If a clinic can understand how many individuals are entering and when they're entering, then they can schedule the day slightly better. Staff scheduling, setup on the rooms, break periods—it all relates back to that.
But just because it’s structured doesn’t mean it works well for everyone. In the city of Boston, the average wait time to get a doctor’s appointment is 72 days. That’s over two months of waiting—for care you might need today.
The general principle of employing appointments is to eliminate that unpredictability. No one enjoys being stuck suddenly, particularly in healthcare, where the consequences are greater than in most settings. But let's be honest, just because it's scheduled does not always translate to it being seamless.
Here’s how appointments help:
Prevents the day from going completely off track
Aids in spreading out patient flow (at least in theory)
Provides an easier way to prevent staff burnout
Provides individuals with something tangible rather than "just wait"
You might also like - How Appointment Scheduling Reduces Administrative Burden in Local Government Agencies
The Problems with Appointments
Appointments are meant to be orderly, but in life, not everything goes as it should. Time doesn't always cooperate with the schedule, and once even the little things go wrong, the entire day can take a turn for the worse.
-
Late patients
All it takes is a single late individual to disrupt the entire queue. Doctors take longer to see patients, others wait longer, and it is difficult to catch up once that delay begins adding up.
-
Appointments taking longer or shorter than planned
Not all check-ups fit into a tidy time frame. Some patients require more care, some require only a brief check. But the schedule remains set, so either someone waits or time simply gets wasted.
-
Schedule gaps filled by no-shows
A no-show appointment is an unfilled time slot that nobody else can see at the last minute. That's lost time and lost money, particularly when it happens repeatedly.
A study about patient no-shows found that 44% of participants skipped appointments because they felt disrespected by the healthcare system. Many patients believe their time, opinions, and feelings aren’t valued—which makes them less likely to come back at all.
-
Abuse of after-hours care
Emergencies are not concerned with schedules. But when physicians are fully scheduled, urgent walk-in patients must either wait too long or be shoehorned into already busy schedules.
Are Walk-Ins Really That Bad?
There's the old assumption that walk-in appointments are chaotic, stressful, and difficult to handle. Individuals see crowded waiting rooms, long waiting periods, and frazzled staff juggling too many tasks at one time. But that's not as much about what is walk-in appointment—it's more about inefficient systems behind them.
In fact, walk-ins are not the problem. It's a lack of equipment and disorganization that create the mess. Done correctly, walk-ins can provide more flexibility and more effective care than appointments.
Here's what typically goes wrong:
No visible means of patients checking in or signing in
Workers cannot view who is waiting or for what
Guests were not informed of when they could expect their turn to come.
But properly managed, walk-ins are an asset:
Patients are more independent with self-check-in facilities
Employees can triage and rank on the fly
Live updates alleviate anxiety and enhance experience
So no, walk-ins are not the villain. Poor queue management is. With the right attitude, walk-in vs appointment isn't even an issue—it's just good service design.
How to Make Walk-Ins Work Better
Walk-in systems don’t have to feel like a mess. When done right, they can actually make the flow smoother than scheduled appointments. Here’s what helps.
1. Use self check-in kiosks.
Instead of standing in line just to tell someone you’ve arrived, self check-in gives patients the freedom to log in themselves as soon as they walk in. It cuts down the chaos at the front desk and also makes the whole process feel a bit more personal and less clinical.

Patients can type in their name, choose why they are there, and even provide additional information if necessary—directly from a tablet or kiosk.
Assists in preventing long front-desk queues during peak hours
Decreases paperwork and accelerates first contact
Provides patients with control and privacy upon check-in
2. Send updates via SMS or display screens.
The individuals that wait with no sense of timing get frustrated quickly. Simply informing them where they are in the queue or how long it will take can totally change their disposition. A basic display screen at the lobby or a text notification is enough.

Qminder provides updates straight to patients' phones and also displays queue information on screens, so no one's left guessing.
Keeps patients apprised without having to ask staff
Decreases perceived wait time by establishing expectations
Makes things seem to be run efficiently even when it's hectic
3. Let patients choose services and give info upfront.
When walk-ins can indicate what they're there for at check-in, it's one step ahead for your staff. Whether someone is there for a flu shot or requires blood work, knowing that ahead of time helps in quicker routing and less bottlenecks.
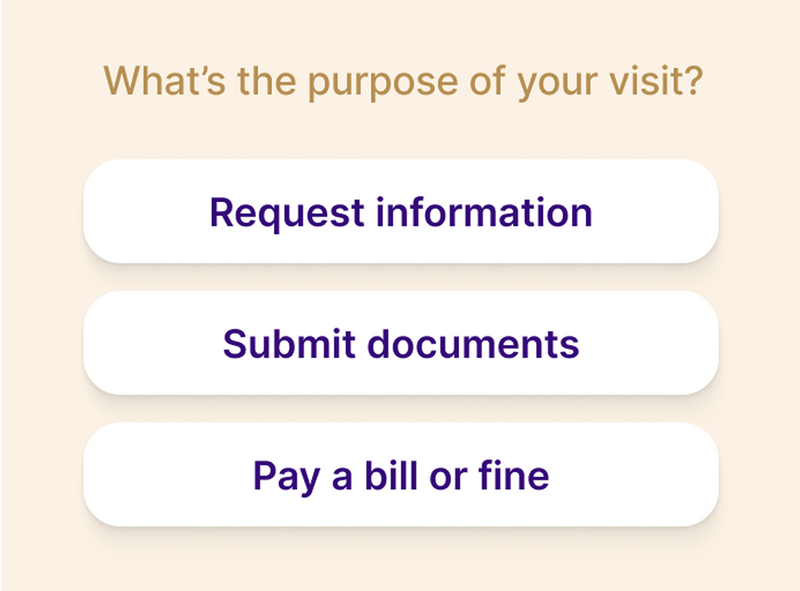
An appointment scheduling software’s check-in process allows individuals to select their service and respond to a couple of brief questions, which serves to divide the crowd into context queues.
Accelerates triage and reduces wasted back-and-forth
Streamlines different departments' management
Prevents complicated visits from delaying simple ones
4. Use Data to Predict Peak Times and Plan Resources
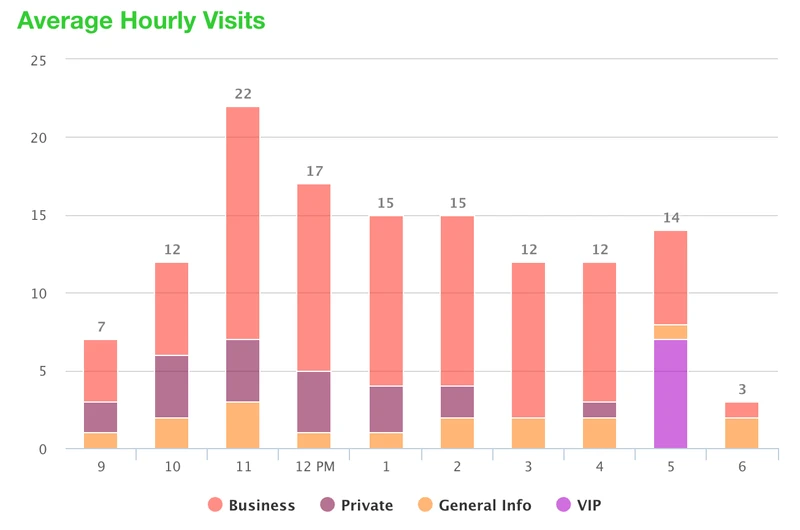
Understanding when walk-in traffic usually peaks can help avoid those frantic last-minute rouse processes. Using the analytics data to examine check-in times, wait times, and service volumes will begin the process of forecasting your busiest hours.
Such data gives you the power to plan ahead - you may wish to change shift plans, open additional service desks or think in advance about staffing certain departments. Rather than reacting to a crowd, you can proactively plan for them.
Spot daily or weekly traffic patterns
Match staffing levels to actual demand
Improve overall flow during high-pressure periods
5. Track everything in one place with a real-time dashboard.
A dashboard that shows who’s waiting, what they need, and how long they’ve been waiting helps your team stay one step ahead. It gives staff real-time visibility into patient flow and service demand, making it easier to manage walk-ins without feeling overwhelmed.
Qminder’s Service Dashboard brings all this together in one screen—so your team can triage faster, prioritize better, and route patients more efficiently.
Helps manage high volumes without losing track
Gives staff a real-time pulse on patient flow
Makes triage and routing decisions quicker and easier
Walk-In vs Appointment: Which One Wins?
It's really a matter of the arrangement. The walk-ins are a godsend some days—patients come in, get taken care of, and they're gone. Appointments are what save the day on others. Reality is, both have their drawbacks and advantages, and the best outcome is usually found when using them together.
Appointments provide the structure. You have a sense of who's arriving, about when, and how to schedule the staff accordingly. But actual life doesn't always adhere to a grid. People cancel out. Some fail to appear. Others walk in with unscheduled emergencies on their minds.
Patient cancellations alone can cost clinics up to $2,500 in lost revenue each month, with some practices reporting losses as high as $7,500 per month. Without a way to fill those gaps quickly, that’s revenue gone for good.
That's where a hybrid model becomes more sensible. Let appointments schedule the day, and let walk-ins take up the slack. A queue system such as Qminder assists both in managing—without overloading staff or leaving patients in the dark.
Here’s a table to make things easier to compare:
Feature / Factor | Walk-In Appointment | Scheduled Appointment |
Flexibility | High – patients come when needed | Fixed – locked into specific times |
Patient Experience | Convenient, but risk of waiting | Predictable, but strict |
Operational Planning | Can be messy without a system | Easier to plan staffing |
Handling No-Shows | Not an issue | Can leave empty slots |
Urgent Care Cases | Easier to accommodate | Might delay or bump others |
Tech Support | Works better with tools like Qminder | Also benefits from automation |
Rather than arguing walk in vs appointment, the smarter option may be: how do you get the best of both?
A well-run walk in appointment flow with digital check-ins, live updates, and patient information upfront makes a big difference. Systems like Qminder handle the chaos without needing a full operations overhaul.
Also read - Walk-in vs. Appointment Scheduling: Choosing the Best Approach
Why More Hospitals Are Choosing Walk-Ins
Hospitals are finally beginning to reconsider how they manage patient flow. It's not always about having a fixed schedule—sometimes it's about being prepared when people are ready for you. That's where walk-ins fit in. They're not new, but when combined with the right tools, they've begun to feel much more manageable.
Unlike old-school schedules that disintegrate the moment one cancels or is late, walk-ins leave more space to improvise. And when you are employing tools like Qminder in managing the flow, walk-ins become much more manageable.
Here's why hospitals are leaning into walk-ins:
-
Faster service overall
Patients don’t always have to wait for the next “available” appointment slot—especially when the line is moving in real time.
-
Patients feel more at ease
No need to wait weeks. They come in, get help, and leave without having to play calendar tag.
-
Smarter staff allocation
When the system shows exactly who’s waiting for what, it’s easier to shuffle tasks and avoid bottlenecks.
-
More flexibility for urgent care
Staff can prioritize based on need, not just appointment order.
-
Better flow during peak hours
Walk-ins help fill unused gaps and make use of every available minute without overloading anyone.
It’s not about picking walk-ins over appointments completely. It’s about giving patients options—and giving hospitals more control.
Title:
Make Walk-Ins Work—Without the Chaos
CTA Text:
See how Qminder helps hospitals and clinics manage walk-ins with real-time updates, self check-in, and smoother patient flow—no appointment needed.
Rethink How You Handle Patient Flow
Whether you're leaning towards scheduled care or need the freedom of walk-ins, it's about juggling both with the proper equipment. Appointments may plan ahead, sure—but when life gets messy, walk-ins can keep things afloat. The best outcome results from mixing both, with a system that updates patients and staff accordingly.
Qminder's patient check-in system facilitates hospitals in managing walk-in appointments seamlessly, with functionalities such as self check-in, real-time messagings, and insights into data. It's designed to assist the workflow—not hinder it.
Try Qminder free for 14 days and see how it can transform your hospital experience.
Yes, most contemporary queue systems such as Qminder can accommodate multiple languages on kiosks and on-screen. This can be made easier for non-native speakers of the primary language.
Small things such as open wait-time communication, seated ergonomic arrangements, and warm greetings can make a big difference. Real-time notification also eliminates uncertainty.
Hospitals can monitor average wait times, peak hours, no-show percentages, and service demand per department. All this data assist in more efficient staffing and planning.