Nobody likes waiting in a hospital lobby, especially when they’re already worried or in pain. Long patient waiting times are one of the biggest frustrations people face when visiting a hospital or emergency room.
And while medical needs can’t always be planned, knowing when to go can make a noticeable difference.
According to a report, the average wait time in Canadian emergency rooms is over 2 hours and 12 minutes, with some hospitals far exceeding that.
This guide breaks down the common “best” and “worst” times to visit, including when it’s typically the worst time to go emergency room.
What Influences Hospital Wait Times?
Several factors affect how long patients wait at hospitals. These include how many staff are available, when people tend to visit, and how well the hospital’s system is set up to manage the flow.
Staffing Levels
Hospitals have fluctuating staffing levels throughout the day. Typically nights, weekends, and holidays often have fewer physicians and nurses available, which delays everything from check-in to treatment. In the case of emergency departments, it is more likely that these delays are exacerbated when several patients come in simultaneously.
Volume Patterns
Hospitals also have volume patterns. Some times of the day breed larger crowds. Mornings tend to be crowded because most patients prefer to start their day early. The same can be said for the day following weekends or holidays, as patients that were waiting now show up all together and build queues and wait times.
Internal Inefficiencies
Even in the presence of staff, the internal delays can still persist. Patients still have to endure the delays that add up, such as manual check-ins, vague directions, and poor transfers among departments. Hospitals may not employ a queue system or real time tracking; therefore, these delays are allowed to build quietly with no efficient flow through the hospital, all of these things slow the patient process down.
The Worst Times to Visit a Hospital
Not all hours are equal in a hospital. Some times are slower, more crowded, or harder to navigate. Knowing when these peaks happen can help you avoid long delays and added stress. Here are the times when patient waiting times tend to be at their worst:
1. Nights and Weekends
Hospitals don’t keep the same pace after regular hours. Nights and weekends usually run with fewer doctors, fewer nurses, and fewer support staff. If more patients walk in than expected, delays become harder to avoid. That doesn’t mean the care isn’t there—it just takes longer to reach you.
One study in the Journal of the American College of Cardiology found that heart attack patients admitted at night had slightly lower survival rates compared to those treated during the day. It’s not about the quality of care. It’s about how fast things can move when teams are stretched thin.
Some of the common reasons wait times go up during these hours:
Most departments have fewer people on shift
Some areas may be closed until the next morning
Lab and imaging results can take longer to come back
On-call specialists may not be in the building
Staff may need to prioritize urgent cases over everything else
2. Holidays and Long Weekends
Holidays usually stretch hospitals thin. Some staff are off, departments may run shorter hours, and the ones on duty often have more to manage than usual. Patients feel the difference. Delays get longer, communication gets slower, and it’s easy for things to fall behind.
Experienced staff may also be off during this time, which leaves fewer people to guide or troubleshoot when things don’t go as planned.
A few things that add to the wait during holidays:
Fewer doctors and nurses on shift, especially in non-emergency roles
Slower response times from lab, imaging, or admin teams
Higher patient stress due to holiday plans or travel-related issues
Less direct oversight from senior or specialized staff
More patients choosing to delay care until after the break, which crowds the days right before and after
3. The July Effect
July is when teaching hospitals bring in new interns. It’s the start of their real clinical work, so they’re still learning how to handle cases, work with systems, and follow hospital routines. They’re not on their own, but that learning curve can slow things down.
Some studies have shown a slight increase in errors during this time. Others say there’s no real impact. But anyone who’s worked in a hospital knows the shift is noticeable, especially in departments that rely on speed and coordination.
What can happen during this period:
Interns take longer to make decisions or complete tasks
There’s more back-and-forth between junior and senior staff
Orders and notes may need extra checking before they’re approved
Small delays can add up if the team is still finding its rhythm
If your visit isn’t urgent, it might be better to avoid the first few weeks of July in a teaching hospital. Things usually settle down once the teams get into a routine.
4. Right after a major local event
Major events like sporting events, concerts, and city festivals can put more patients in neighboring hospitals (not always because they're emergencies). Some patients may not feel the need to seek care until the festival is over, or they'll show up after minor injuries or even heat exhaustion. Either way, it adds to the volume.
Here are a few things to consider about timing right after a significant local event:
There could be an unexpected increase in patients
Staff may be already dealing with volume
Delays are especially long for patients who are not in an emergent situation
Triaging to getting treated (transport, parking, and check in) can take longer
If you are not in a rush to go in, be sure to check what is happening in the area first. A few hours can make a big difference.
Are There Best Times to Visit a Hospital?
While there’s no perfect time to visit a hospital, some hours are clearly better than others. Fewer patients, more staff, and smoother operations can make a big difference. Below are the time windows when hospitals usually run more efficiently and patient waiting times are shorter:
1. Early Weekdays
If you have some flexibility, early weekdays are usually your best bet. Mondays through Wednesdays tend to run smoother. Staff are fresh, departments are fully staffed, and most systems are back to normal after the weekend.
There’s also less foot traffic compared to the end of the week, which helps move things along faster.
Why early weekdays work better:
More staff are available and not stretched thin
Support services like labs and imaging run at full pace
Fewer delays from weekend backlog
Specialists and follow-up services are easier to access
You won’t always get to choose, but if you can, this window is often the most efficient.
2. Late Mornings and Early Afternoons
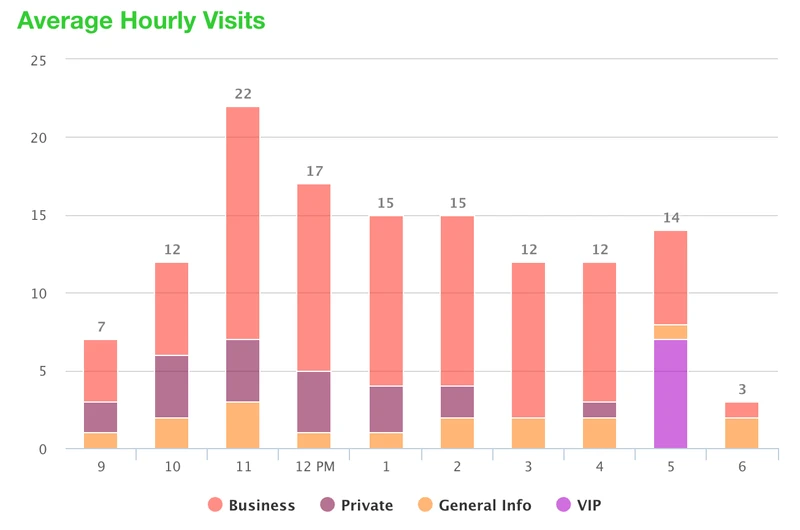
If you are looking to avoid the typical crowd, mid-day is usually your best chance. By the time it is late morning, the first wave of patients has been seen and they have not yet begun their second wave of patients that begins after 12:00 PM. Things go a little smoother during this window of time.
Early morning is very busy because of the overnight cases, or because patients arrive right when the doors open. Typically, late afternoons feel like time is standing still, as staff continue to finish or shift staff begins to change for the day.
Here’s why mid-day works better:
You avoid the early rush and the late slump
Staff are in rhythm and not as stretched
Wait times for labs, imaging, and check-ins are usually shorter
Fewer chances of being caught in last-minute delays
It’s not a fix for every visit, but when you have the choice, this window makes the experience a little smoother.
3. Midweek Over Mondays or Fridays
Typically, Mondays are always busy. We build up a bit of a weekend backlog, plus walk-in patients and people who have been waiting to get things set up or finished. Fridays can feel just as busy, but for different reasons, as many will try to get in before the weekend or tie up loose ends on things they have been delaying. Of course midweek is a little bit more steady and balanced. There is usually a better flow during the day, and not as many patients in a rush.
Why midweek works better:
Mondays come with leftover weekend cases
Fridays bring in last-minute visits and weekend prep
Tuesday through Thursday often see steadier flow
Staff are less likely to be pulled in too many directions
If you’re scheduling something that’s not urgent, aim for the middle of the week. It’s quieter and less chaotic.
4. During Non-Flu Seasons
Hospitals stay busier during flu season. More people show up with fevers, coughs, or breathing trouble, and that makes everything take longer. Even if your case isn’t related, you end up waiting behind the rush.
If it’s something that can wait, it’s better to go outside the winter months. The difference in wait time can be noticeable.
Here’s what changes during flu season:
Emergency rooms fill up faster
Staff have more patients to handle at once
Basic tests and rooms may take longer to get
You’re also more likely to sit near someone sick
It’s not always avoidable, but if your visit is planned ahead, choosing a quieter season helps things move smoother.
How Hospital Queue Management Systems Can Help
A smart patient check-in system like Qminder does more than show a number on a screen. It shapes the entire visit, trims patient waiting times, and gives staff clear data to reduce waiting time day-to-day and over the long run.
Real-Time Queue Management
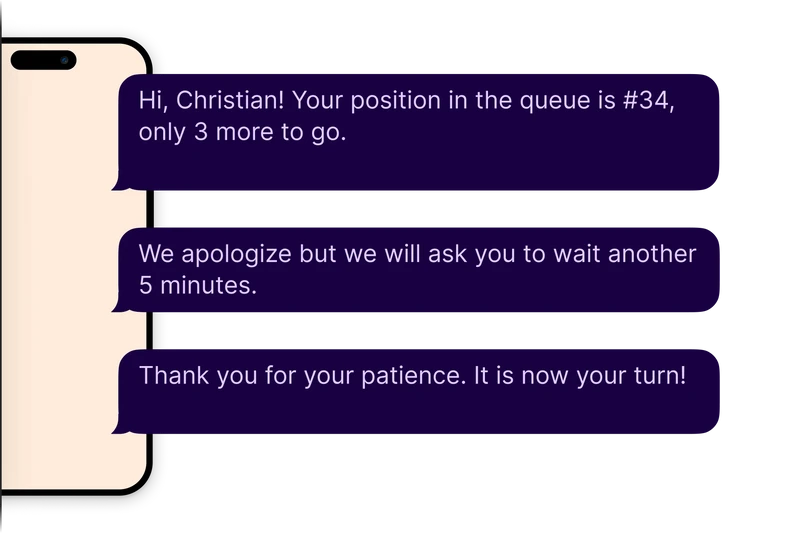
Patients see their place in line on a waiting room TV or on their phone. Knowing what comes next eases stress and cuts down repeat questions at the desk. Staff get a live view of every queue, which lets them shift tasks before a backup turns into the worst time to go emergency room for someone in pain.

Why it works
Live updates keep patients informed and calmer
Staff can move people between services in seconds
Sudden surges are easier to spot and handle
Replacing Sign-In Sheets with Self-Check-In
Paper sign-in slows everything. A self check-in kiosk or a quick tap on a mobile link signs patients in, verifies details, and sends them straight to the right queue. The front desk spends less time on forms and more time on care.

Benefits
No crowded line at a single counter
Details are legible and complete every time
Patients move to the next step without waiting for a call-out
Data Collection and Forecasting
Every visit leaves a time-stamp. Over weeks and months, that data turns into a clear picture of peak hours, busy seasons, and staff load. Managers can plan schedules that fit real demand instead of guessing.
What hospitals gain
Accurate forecasts for staffing and rooms
Quick reports on average wait by service or day
Early alerts when patient waiting times creep up
Better Walk-In Experience
Virtual queueing lets walk-ins join the line from a kiosk, a link, or even the parking lot. Names appear on the screen, not ticket numbers, so staff greet people instead of yelling codes across the room.
Results
Less crowding and more personal service
Patients wait where they feel comfortable and get an SMS when it’s their turn
Overall flow stays smooth even when walk-ins spike
Make Every Time the Right Time
Long wait times at hospitals are sometimes unavoidable, but by knowing when to go, and what to expect, you can at least help reduce your wait time and improve your experience.
Avoiding weekends and holidays and simply understanding how staffing patterns cause waiting time delays can provide a significant improvement in your experience with just small changes in timing. However, timing alone is not enough.
Modern patient queue management softwares alleviate confusion within hospitals, reduce frustration for waiting patients, and increase predictability within each visit. This is where Qminder comes into play. Qminder is designed for healthcare teams wanting useless workflows and shorter patient waiting times.
See how Qminder can help your hospital reduce wait times and improve overall patient care.
Yes, they can. Many mobile apps allow for pre-check in, allow patients to see accurate, real time queue updates and allow notifications when it is a patient's turn. Meaning less crowding and more predictable visiting.
Not always. Some hospitals still have manual systems and miss patterns in patient flow. Those hospitals using a digital queue system (like Qminder's service) will be able to see trends in their patient flow and have data to utilize in planning.
It depends on location and time. Private hospitals may have fewer patients at any given time but that does not mean it will reduce wait times unless a queue system is used.